NHS will get better blood and organ matching data from Our Future Health partnership
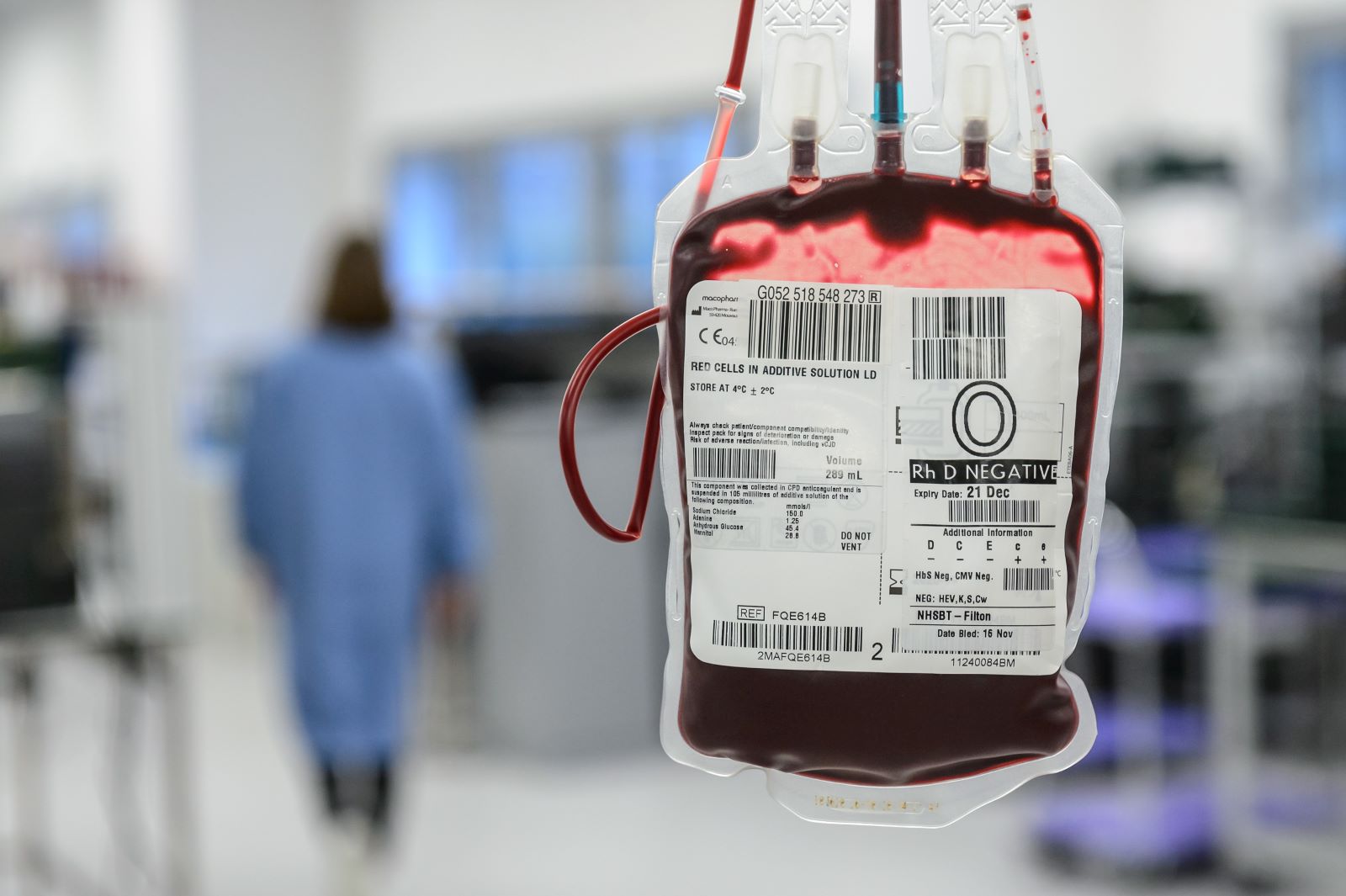 Blood donors in England can now give a sample to the UK’s largest health research programme as they give blood.
Blood donors in England can now give a sample to the UK’s largest health research programme as they give blood.
Donors are being invited to give a sample to Our Future Health, which aims to transform the prevention, detection and treatment of conditions such as dementia, cancer, diabetes, heart disease and stroke.
In return, NHS Blood and Transplant will get future access to the donor’s blood, platelet and tissue type genetic data, which will allow for better matching of blood transfusions and stem cell and organ transplants.
This week, 207 people will be giving the first samples as they donate at sessions run by four mobile blood donation teams covering parts of Kent, Bristol, Leeds and Wiltshire.
Participants will give blood as normal but during the donation a small amount of blood will be diverted into a sample bag and later sent to Our Future Health.
NHSBT aims to roll out sampling to all of its 24 donor centres and 48 mobile teams by the end of 2023. The ambition is to recruit up to 450,000 blood donors into the programme over the next five years.
Donors will receive invites with a personal link to a web page where they complete a consent form before coming to the session. Donors will not be able to give samples on session until they have received personal invites and completed consent forms. (1)
How will this partnership help?
Our Future Health will carry out detailed tests on the blood for its research programme, which will include testing the extended blood, platelet and tissue types. NHSBT will then have future access to the blood, platelet and tissue typing genetic data, though not other data.
There are currently around 800,000 blood and platelet donors and more than 28 million people have opted into the NHS Organ Donor Register. However, the complexity of blood and tissue types mean that suitable donors cannot always be found. There are 354 known blood types (or antigens) and more than 36,000 known HLA types (or tissue types).
Finding matches can be a particular problem for people of black Afro-Caribbean and Asian heritage.
For example:
- Sickle cell disorder is more common of black heritage. Around 17% of people with sickle cell have developed antibodies because blood transfusions could not be completely matched, meaning it can be difficult or even possible to find matching blood in the future.
- Asian people wait five months longer for a kidney transplant, due to the shortage of matching donors.
- Caucasian people have an up to 90% chance of finding a stem cell match on the NHS British Bone Marrow Registry but for people from black, Asian and mixed ethnic backgrounds, they have a 40% chance or less.
The data provided to NHSBT will help provide better match products. We anticipate particular benefit in the future for kidney transplant patients by providing blood for transfusions that do not raise antibodies to their transplanted kidney. The antibodies make it harder to find matching blood for the future and increase the risk of the organ being rejected.
Out Future Health is seeking to recruit up to five million volunteers from across the UK through various recruitment channels to create one of the most detailed pictures ever of people’s health. With this information, OFH said researchers will be able to develop new ways to prevent, detect, and treat diseases.
There are thousands of people like me hoping for a miracle match.
 Alisha Gorkani, aged 24, from Sidcup in the London Borough of Bexley, a solutions advisor for a tech company, has spent almost six years waiting for a matching kidney transplant.
Alisha Gorkani, aged 24, from Sidcup in the London Borough of Bexley, a solutions advisor for a tech company, has spent almost six years waiting for a matching kidney transplant.
She had juvenile nephronophthisis, which caused scarring of her kidneys and kidney failure as a teenager.
Alisha received a living kidney donation from her mother but the organ was rejected and she developed numerous antibodies during the treatment.
She now receives dialysis over 3-4 hours, every Monday, Wednesday and Friday, on the site of Queen Mary Hospital in Sidcup, in a unit operated by Guy's and St Thomas' NHS Foundation Trust.
Alisha said: "As I have had a transplant before my body has created a lot of antibodies which provides extra challenges so I could be waiting a very long time.
"I try to make the best of things but waiting for a kidney and being on dialysis is incredibly hard.
"It does give me hope that people like my could have better matched blood and organs in the future. There are thousands of people like me hoping for a miracle match."
 Deborah Allison, 57, a retired NHS midwife and manager from Gravesend, is one of those giving a sample as she donates blood today [July 19] in Gravesend.
Deborah Allison, 57, a retired NHS midwife and manager from Gravesend, is one of those giving a sample as she donates blood today [July 19] in Gravesend.
She said: "As an NHS manager, my team have benefitted from ongoing medical research, hence my interest in Our Future Health.
"And as a midwife, I cared for women who bled excessively at delivery and required many units of blood – who can I not contribute in return?
"Now that I am retired, this project keeps me linked into helping the NHS in the future."
Tim Smith, 66, from Southfleet in Kent, a retired manager, is one of the people giving a sample to Our Future Health as he donates blood for the 51st time, at a session in Gravesend today [July 19].
 Tim said: "My motivation is that it’s just that it’s a worthwhile thing to do. I can play my part to help others.
Tim said: "My motivation is that it’s just that it’s a worthwhile thing to do. I can play my part to help others.
"It could also help me one day, because you never know what will happen in the long term.
"And it’s very positive to know my blood donations could be matched even better to help other people."
Press Release Notes
- NHSBT blood donation sessions will not be used for the general public to give samples to Our Future Health. General members of the public aged over 18 can sign up to take part of Our Future Health by signing up online, completing an online health questionnaire, and booking a short appointment at one of the Our Future Health Clinics.