Kidney transplant patients to get blood matched for white blood cells in new programme
 Kidney transplant patients will get blood transfusions matched not just for red blood cells but also for the donor’s tissue type, to help reduce the formation of immune system antibodies and transplant rejection.
Kidney transplant patients will get blood transfusions matched not just for red blood cells but also for the donor’s tissue type, to help reduce the formation of immune system antibodies and transplant rejection.
The programme is going live this month. NHS Blood and Transplant will match the blood at a specialist Histocompatibility and Immunogenetics laboratory in Colindale, London, and supply it for selected pre and post-transplant patients at Hammersmith Hospital, part of Imperial College Healthcare NHS Trust.
If the pilot programme proves successful and a national matching programme is then rolled out, it could significantly reduce the time spent on the waiting list for a transplant and help prevent premature transplant failure. NHSBT data analysis shows current transplant graft survival and patient survival are significantly higher for patients who do not receive transfusions.
How tissue typing helps
Human leucocyte tissue antigen (HLA) typing, also called tissue typing, is not normally needed for most blood transfusions. The creation of HLA antibodies against unmatched transfused white blood cells usually has no consequence. However, in transplant patients, these HLA antibodies may harm the transplanted kidney because they consider it to be ‘foreign’.
Around 2 out of every 5 kidney transplant patients need blood transfusions before or after transplant. Transfusions save lives but they are also associated with double the risk of losing the transplant, according to NHSBT statistical analysis, due to the formation of HLA antibodies.
Additionally, in people waiting for a potential transplant, one in four have a delay to finding a match due to transfusion antibody formation with some patients never being offered a suitable match.
A successful programme and wider roll out would not just provide better patient outcomes also save the NHS money – if a patient needs to return to hospital dialysis that costs the NHS around £20,000 to £33,000 a year.
The potential wider roll out is now possible thanks to advances in the ability to DNA test blood large scale. NHSBT has recently started to use the new Axiom array genotyping test, developed by the Blood transfusion Genomics Consortium (BGC), which offers the ability to potentially HLA type many more donors, as it is cheaper than current testing methods.
Should the programme prove to be a success, NHSBT estimates it will need at least 130,000 blood donors to be HLA typed to make the supply of fully HLA-matched red cells routine for kidney transplant patients. Currently, just under 100,000 donors are typed.
During 2022-23, 2,339 people received deceased donor kidney transplants in the UK. There are currently – as of the end of March – 5,870 people on the kidney transplant waiting list.
Alisha's story
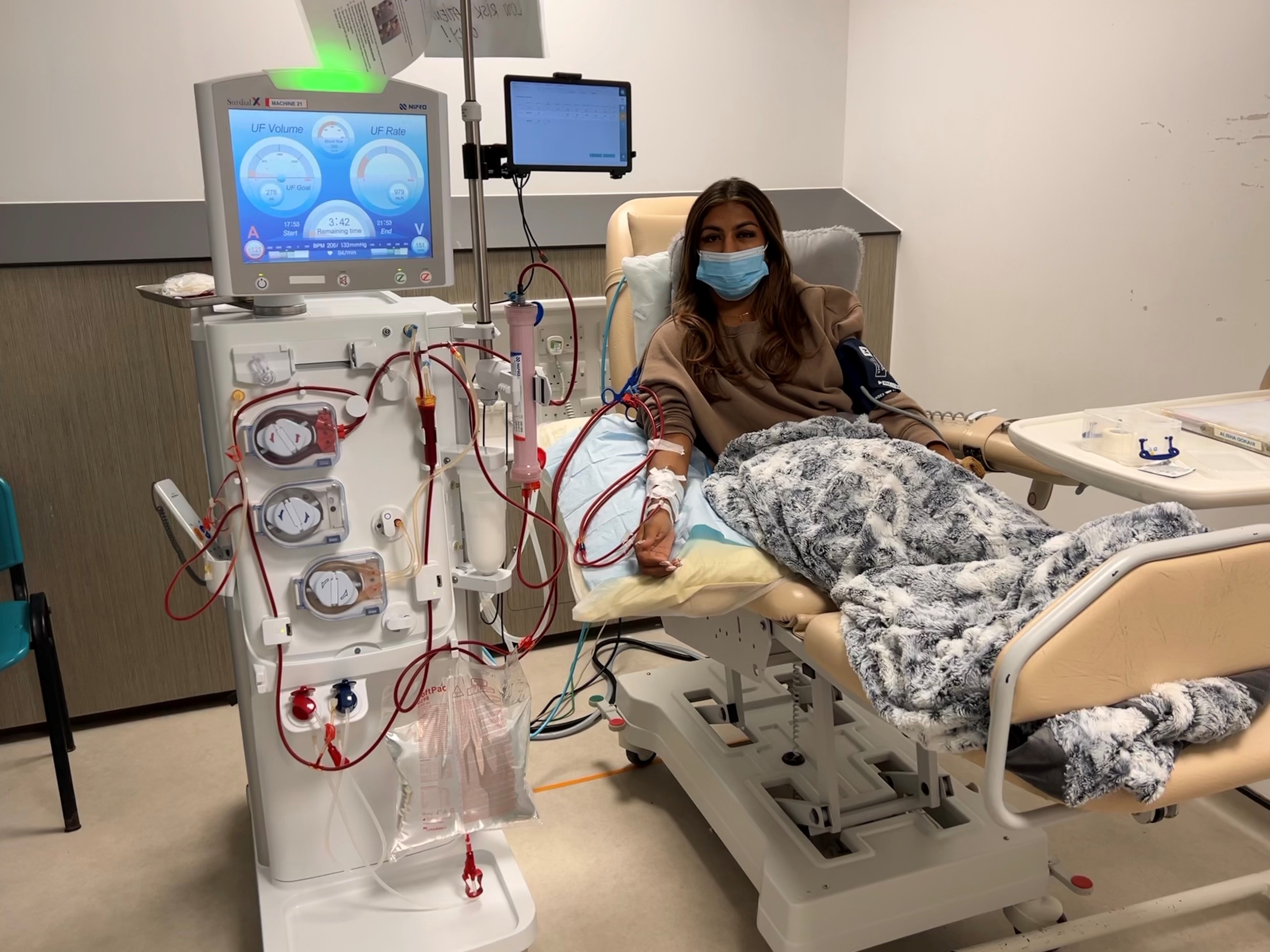 Alisha Gorkani, aged 25, from Sidcup in the London Borough of Bexley, a solutions advisor for a tech company, has juvenile nephronophthisis and has spent seven years waiting for a matching kidney transplant.
Alisha Gorkani, aged 25, from Sidcup in the London Borough of Bexley, a solutions advisor for a tech company, has juvenile nephronophthisis and has spent seven years waiting for a matching kidney transplant.
She has developed antibodies from a mix of blood transfusions and a past kidney transplant.
Alisha said: “I have a lot of antibodies so I could be waiting a very long time. I try to make the best of things but waiting for a kidney and being on dialysis is incredibly hard.
“It does give me hope that people like me could have better matched blood in the future. There are thousands of people hoping for a miracle match.”
Gemma's story
 Married mum of two boys Gemma Louis from Chester-le-Street has waited 11 years for a kidney transplant due to sensitisation from a blood transfusion.
Married mum of two boys Gemma Louis from Chester-le-Street has waited 11 years for a kidney transplant due to sensitisation from a blood transfusion.
The 44-year-old civil servant has chronic kidney disease and needs four hours of dialysis three days a week. “I was told initially my wait would be twice as long as normal, so around six years. I am 11 years in now,” said Gemma.
“I knew I would have a long wait purely because of the antibodies I developed to the transfusion. It’s harder to find a match which won’t be rejected. This programme sounds like it could potentially help people like me in the future. I know people at my unit who are even more sensitised.
“In general, there is still a need for more organ donors. I absolutely think people should join the Organ Donor Register. I think most people would be willing to accept so why wouldn’t you be willing to donate?”